The one-anastomosis gastric bypass, or OAGB, is becoming more widely acknowledged as a particularly advantageous surgical procedure for patients with extreme obesity. This method’s simplified single-anastomosis approach makes it extremely effective compared to traditional gastric bypass, drastically cutting down on both operational time and potential problems.
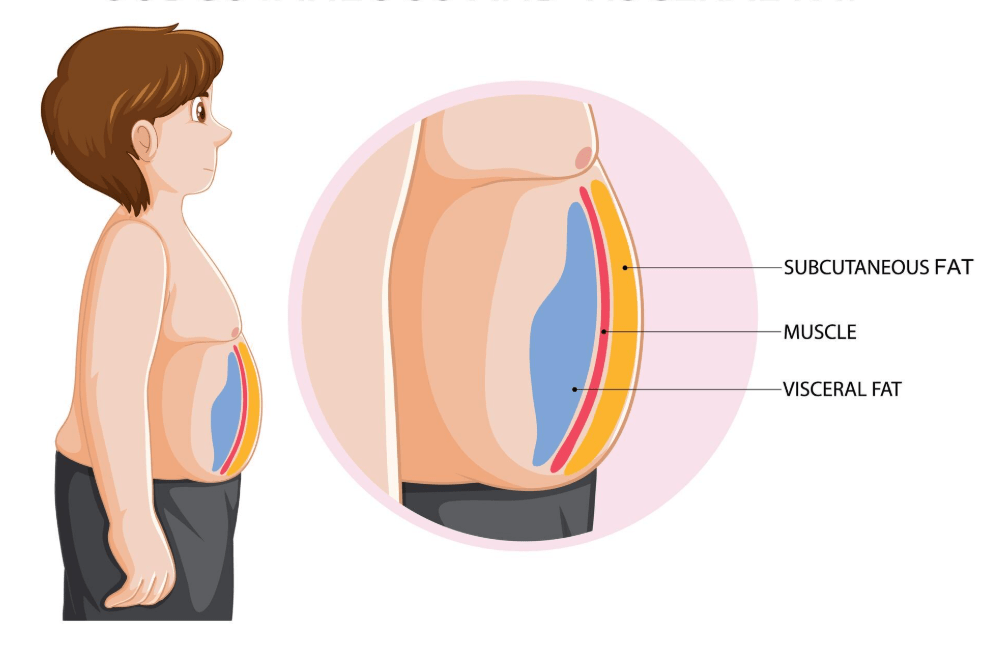
Surgeons produce a long, narrow pouch that resembles a banana by excising a considerable section of the stomach’s outer layer. This anatomical alteration helps patients feel fuller faster by limiting food intake and is incredibly lasting. Moreover, calorie absorption is significantly decreased by redirecting a portion of the small intestine—a dual mechanism remarkably like a two-pronged strategy targeting both hunger and digestion.
OAGB Surgery – Key Information Summary
| Aspect | Details |
|---|---|
| Procedure Name | One-Anastomosis Gastric Bypass (OAGB) |
| Also Known As | Mini Gastric Bypass, Omega Loop Bypass |
| Primary Purpose | Surgical intervention for weight loss and obesity-related health improvements |
| How It Works | Reduces stomach size and bypasses part of small intestine to lower calorie absorption |
| Key Benefit | Encourages early satiety and significantly reduced calorie intake |
| Stomach Pouch Size | Comparable to a banana (larger than traditional Roux-en-Y pouch) |
| Surgical Type | Laparoscopic (minimally invasive using small incisions) |
| Average Surgery Duration | Typically shorter and simpler than traditional bypass |
| Weight Loss Results | 50% to 80% of excess weight typically lost in 18 months |
| Notable Advantage | Only one anastomosis (surgical connection) required, reducing risk |
| Common Complication | Bile reflux (affects approximately one-third of patients) |
| Preparation Required | High-protein, low-calorie diet; avoid NSAIDs; pre-op hygiene instructions |
| Hospital Stay | Minimum one night (may vary based on patient recovery) |
| Post-Op Diet | Begins with liquids and purées, progresses to high-protein solids |
| Long-Term Lifestyle Needs | Daily hydration, protein intake (60–100g), supplements, physical activity |
| Potential Long-Term Issues | Nutrient deficiencies, ulcers, pouch enlargement, iron deficiency anemia |
| Comparison to Roux-en-Y | Equally effective; simpler technique; similar outcomes; fewer incisions |
| Success Rate (Quality of Life) | 86% of patients reported improved or greatly improved quality of life after 92 months |
| Reference Site |
By this reconfiguration, OAGB affects the hormonal balance that controls appetite in addition to changing physical intake. Ghrelin, the so-called “hunger hormone,” has been shown in recent research to decrease after surgery, giving patients a greater sense of fullness. What’s the downstream effect? Particularly in the first six months, patients lose weight more quickly.
When compared to the conventional Roux-en-Y gastric bypass, OAGB has demonstrated exceptional efficiency in comparative tests. Although the latter results in a smaller pouch and necessitates two anastomoses, the weight loss outcomes are generally comparable. OAGB is unique since it is executed much more quickly and requires remarkably few hospital resources.
Interest in minimally invasive procedures increased during the epidemic, especially among people looking for long-term health solutions following months of leading inactive lives. Given that OAGB is laparoscopic, which results in a quicker recovery and less hospital stays, it stood out as a very robust and successful technique.
In addition to being medical, preparation for the treatment is both emotional and educational. Pre-operative discussions that set clear expectations and expose patients to support networks are frequently recommended. Peer-based coaching programs are now available in many hospitals, where post-operative patients mentor those who are just starting out.
Patients eat a low-calorie, high-protein diet for weeks before surgery. Despite its brief duration, this preoperative phase is essential for liver shrinking, which makes surgery safer and easier to handle. Additionally, patients are advised to follow strict cleanliness guidelines and stop taking specific medications.
The experience is meticulously planned on the day of surgery. Every stage has been made as safe as possible, from anesthetic and IV insertion to cozy attire and simple packing. Trocars serve as entry points for laparoscopic instruments during the surgeon’s five to six tiny incisions in the operating room. These are used to precisely attach an intestinal bypass and staple and remodel the stomach.
After surgery, the recuperation process starts with a liquid diet, progresses to puréed textures, and ends with solid, high-protein foods. The goal of this diet evolution is very clear: to enhance muscle mass, promote recovery, and avoid difficulties.
Doctors advise patients to consume 60–100 grams of protein each day, which actively promotes tissue healing and energy stability, by utilizing nutritional science. Hydration becomes an indispensable ally, serving as a protective barrier against ailments such as weariness, kidney strain, and gastrointestinal problems.
Although OAGB is usually safe, bile reflux is still a major worry. This disorder, which affects almost one in three people, causes digestive bile to back up into the esophagus and pouch. In severe cases, the ensuing inflammation can result in disorders like Barrett’s esophagus or cause discomfort.
Patients can lower their risk of reflux by making sensible lifestyle adjustments. Many people have seen a noticeable improvement in their results by eating smaller, lower-fat meals and standing up straight after eating. These benefits are compounded by abstaining from irritants like alcohol and tobacco. When combined with medical surveillance, these behavioral reinforcements form a potent preventative toolset.
Although they are uncommon, serious problems can occur. Bleeding, intestinal obstructions, and leaks at the anastomosis site are early-stage issues. Subsequent complications could include iron-deficiency anemia, ulcer formation, or narrowing of the surgical incision. If dietary discipline lapses, the pouch may eventually stretch, resulting in less than ideal weight reduction.
Public health narratives have changed quickly over the last ten years, and OAGB has established a reputation as a health transformation tool as well as a weight-loss method. The societal impact is noteworthy since Type 2 diabetes, hypertension, and sleep apnea frequently improve after surgery.
Many clinics are currently lowering cost barriers and increasing accessibility to OAGB through smart partnerships with wellness programs and insurance. More patients are coming forward to use this cutting-edge technique to regain their health as costs become more affordable.
It is impossible to exaggerate the emotional shift that occurs after OAGB. More than 85% of patients report an improved or significantly improved quality of life in follow-up studies. Improved mobility, better-fitting clothes, and a renewed sensation of control are all reflected in the mirror.
The stigma has also been lessened by accounts of famous people who have had comparable operations. Public personalities have encouraged people to put their health above doubt by candidly expressing their challenges and victories. It is especially positive that there is a cultural movement toward acknowledging medical intervention as a means of empowerment.
